For the last 14 years, ophthalmologist Dr Tim Henderson has been delivering eye care services where others dare not tread.
As director of eye health at the Alice Springs Hospital, Tim is the only ophthalmologist in the region for tens of thousands of people, many of whom live in remote communities across the red centre of Australia.
“Most people think I’m nuts,” Tim says, “but despite the many and varied challenges, this place grows on you and my work is extraordinary, fascinating and rewarding and exasperating all at the same time.”
Having grown up in central Africa as the child of medical missionaries, Tim concedes that he has perhaps been better placed than most to deal with the unique challenges and conditions that his job demands of him every day.
“I really went in with my eyes wide open,” he says. “There are so many issues and challenges in a place like this that you would never encounter in a normal medical setting.”
Such challenges include competing with acute health needs in a stretched public health system, short-term funding models that make it difficult to deliver sustainable, more efficient eye health programs, and cultural issues in local Aboriginal communities, which often mean that other things such as “sorry business” take precedence over someone getting eye surgery for which they might be scheduled.
Unfortunately, the result is that eye conditions such as trachoma and cataracts are still prevalent in these communities, and diabetic retinopathy is a growing issue.
“The thing governments really need to understand is that investing in eye health is one of the most cost-effective things you can do,” Tim says. “It delivers a higher quality of life, ensures people’s independence and has an overall high positive return.
“If we were able to get longer-term funding for programs, we’d really be able to deliver high-quality eye care to large parts of the population.”
On top of his work at Alice Springs Hospital, Tim makes up to 40 visits to remote Indigenous communities each year, usually flying in to these small settlements of 300-500 people to do specialist eye team visits.
“We try to do work remotely because people in these communities often can’t or don’t want to come to Alice Springs, so will live with debilitating eye conditions rather than get treatment.
“But meeting people on their homeland, and building long-term relationships, is also important, as it is an expression of respect and serves as a basis for the trust required to offer and deliver the eye health services required.”
To ensure he avoids professional isolation, Tim works closely with a network of specialist eye doctors and outreach workers around the country, so that together, they ensure patients receive the best care possible close to home.
“Having a team of competent, experienced colleagues who can provide specialist expertise when needed really makes all the difference,” he says.
“It’s great to have them come to the hospital and help out with sub-specialty clinics. They get great training here too, because they are often presented with complex cases.”
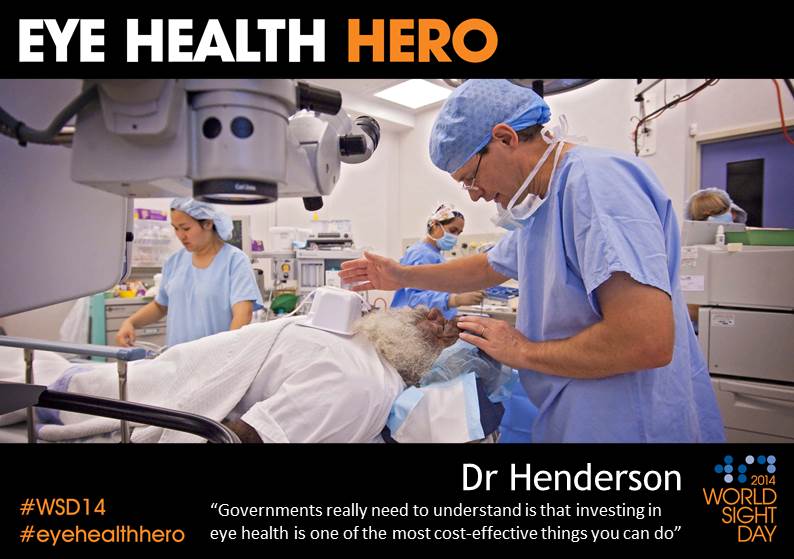
Tim’s favourite part of the job is performing eye surgery, so he particularly looks forward to the operating-blitz weeks at the hospital.
“I love the weeks we do surgery here—as I’m really a surgeon at heart.
“Successful surgery requires craftsmanship and I get great satisfaction from completing a technically difficult task with precision and, if possible, making it look easy so it belies the complexity.
“Teaching surgery to the eye surgeons in training and seeing them grow in confidence is also very satisfying.”
“When everything goes right in such a difficult environment, there’s an enormous sense of teamwork and achievement for everyone involved—just getting the patient to the hospital in the first place, having them trust you with the safety of their eye, and then seeing a good outcome, or that we’ve transformed a person’s life.”
Despite the long hours and heavy workload, Tim says he continues to love the life he shares in Alice Springs.
“There is a lot of richness in this place and a strong community spirit—this is part of the reason I’ve stayed.
“But ultimately, it’s just the extraordinary sense of achievement I feel a part of. For me, it’s a privilege to provide such a service.
- Download Dr Henderson’s story in PDF here
- Photo credit: Barry Skipsey/The Fred Hollows Foundation
